Scientific Baby Bone Pictures Bone Anatomy From Birth to Deatb
Bones are an of import part of the musculoskeletal system. This commodity, the kickoff in a two-part serial on the skeletal organisation, reviews the beefcake and physiology of os
Abstract
The skeletal arrangement is formed of bones and cartilage, which are connected by ligaments to course a framework for the rest of the trunk tissues. This commodity, the first in a two-part series on the construction and function of the skeletal organisation, reviews the beefcake and physiology of bone. Understanding the structure and purpose of the bone allows nurses to understand mutual pathophysiology and consider the virtually-appropriate steps to improve musculoskeletal health.
Citation: Walker J (2020) Skeletal organization 1: the anatomy and physiology of bones. Nursing Times [online]; 116: 2, 38-42.
Author: Jennie Walker is principal lecturer, Nottingham Trent University.
- This article has been double-blind peer reviewed
- Scroll downwards to read the article or download a impress-friendly PDF hither (if the PDF fails to fully download delight try once more using a dissimilar browser)
- Read part 2 of this series here
Introduction
The skeletal system is composed of bones and cartilage connected by ligaments to form a framework for the remainder of the body tissues. There are two parts to the skeleton:
- Centric skeleton – basic along the centrality of the torso, including the skull, vertebral cavalcade and ribcage;
- Appendicular skeleton – appendages, such as the upper and lower limbs, pelvic girdle and shoulder girdle.
Function
Too as contributing to the body's overall shape, the skeletal system has several key functions, including:
- Support and movement;
- Protection;
- Mineral homeostasis;
- Blood-jail cell germination;
- Triglyceride storage.
Support and movement
Bones are a site of attachment for ligaments and tendons, providing a skeletal framework that can produce movement through the coordinated use of levers, muscles, tendons and ligaments. The bones act equally levers, while the muscles generate the forces responsible for moving the basic.
Protection
Basic provide protective boundaries for soft organs: the attic around the brain, the vertebral column surrounding the spinal string, the ribcage containing the heart and lungs, and the pelvis protecting the urogenital organs.
Mineral homoeostasis
Equally the main reservoirs for minerals in the body, bones contain approximately 99% of the body's calcium, 85% of its phosphate and 50% of its magnesium (Bartl and Bartl, 2017). They are essential in maintaining homoeostasis of minerals in the claret with minerals stored in the bone are released in response to the body'due south demands, with levels maintained and regulated by hormones, such as parathyroid hormone.
Blood-cell germination (haemopoiesis)
Blood cells are formed from haemopoietic stalk cells present in cerise bone marrow. Babies are born with only red bone marrow; over fourth dimension this is replaced by yellow marrow due to a subtract in erythropoietin, the hormone responsible for stimulating the production of erythrocytes (red blood cells) in the os marrow. Past adulthood, the corporeality of scarlet marrow has halved, and this reduces further to around 30% in older age (Robson and Syndercombe Courtroom, 2018).
Triglyceride storage
Xanthous bone marrow (Fig 1) acts as a potential energy reserve for the trunk; it consists largely of adipose cells, which store triglycerides (a type of lipid that occurs naturally in the blood) (Tortora and Derrickson, 2009).

Bone composition
Bone matrix has 3 primary components:
- 25% organic matrix (osteoid);
- 50% inorganic mineral content (mineral salts);
- 25% h2o (Robson and Syndercombe Court, 2018).
Organic matrix (osteoid) is made up of approximately 90% type-I collagen fibres and 10% other proteins, such as glycoprotein, osteocalcin, and proteoglycans (Bartl and Bartl, 2017). Information technology forms the framework for basic, which are hardened through the deposit of the calcium and other minerals effectually the fibres (Robson and Syndercombe Court, 2018).
Mineral salts are beginning deposited betwixt the gaps in the collagen layers with in one case these spaces are filled, minerals accumulate around the collagen fibres, crystallising and causing the tissue to harden; this process is chosen ossification (Tortora and Derrickson, 2009). The hardness of the bone depends on the type and quantity of the minerals available for the torso to apply; hydroxyapatite is one of the primary minerals present in bones.
While bones need sufficient minerals to strengthen them, they as well need to prevent existence broken by maintaining sufficient flexibility to withstand the daily forces exerted on them. This flexibility and tensile strength of bone is derived from the collagen fibres. Over-mineralisation of the fibres or impaired collagen production can increment the brittleness of basic – as with the genetic disorder osteogenesis imperfecta – and increase bone fragility (Ralston and McInnes, 2014).
Structure
Os compages is fabricated upwards of ii types of bone tissue:
- Cortical bone;
- Cancellous bone.
Cortical bone
Also known as meaty os, this dense outer layer provides support and protection for the inner cancellous structure. Cortical bone comprises three elements:
- Periosteum (Fig 1);
- Intracortical area;
- Endosteum (Bartl and Bartl, 2017).
The periosteum is a tough, fibrous outer membrane. Information technology is highly vascular and almost completely covers the bone, except for the surfaces that grade joints; these are covered by hyaline cartilage. Tendons and ligaments attach to the outer layer of the periosteum, whereas the inner layer contains osteoblasts (os-forming cells) and osteoclasts (os-resorbing cells) responsible for os remodelling.
The function of the periosteum is to:
- Protect the os;
- Help with fracture repair;
- Attend bone tissue (Robson and Syndercombe Court, 2018).
It as well contains Volkmann's canals, small channels running perpendicular to the diaphysis of the bone (Fig ane); these convey blood vessels, lymph vessels and nerves from the periosteal surface through to the intracortical layer. The periosteum has numerous sensory fibres, then bone injuries (such every bit fractures or tumours) can be extremely painful (Drake et al, 2019).
The intracortical bone is organised into structural units, referred to every bit osteons or Haversian systems (Fig two). These are cylindrical structures, composed of concentric layers of os chosen lamellae, whose structure contributes to the strength of the cortical bone. Osteocytes (mature bone cells) sit down in the small spaces between the concentric layers of lamellae, which are known as lacunae. Canaliculi are microscopic canals betwixt the lacunae, in which the osteocytes are networked to each other by filamentous extensions. In the centre of each osteon is a cardinal (Haversian) canal through which the blood vessels, lymph vessels and nerves pass. These fundamental canals tend to run parallel to the axis of the bone; Volkmann's canals connect adjacent osteons and the blood vessels of the fundamental canals with the periosteum.

The endosteum consists of a thin layer of connective tissue that lines the inside of the cortical surface (Bartl and Bartl, 2017) (Fig i).
Cancellous bone
Besides known as spongy bone, cancellous bone is found in the outer cortical layer. Information technology is formed of lamellae arranged in an irregular lattice structure of trabeculae, which gives a honeycomb appearance. The big gaps betwixt the trabeculae assistance make the bones lighter, and then easier to mobilise.
Trabeculae are characteristically oriented along the lines of stress to help resist forces and reduce the hazard of fracture (Tortora and Derrickson, 2009). The closer the trabecular structures are spaced, the greater the stability and construction of the os (Bartl and Bartl, 2017). Red or xanthous bone marrow exists in these spaces (Robson and Syndercombe Court, 2018). Red os marrow in adults is constitute in the ribs, sternum, vertebrae and ends of long bones (Tortora and Derrickson, 2009); it is haemopoietic tissue, which produces erythrocytes, leucocytes (white blood cells) and platelets.
Blood supply
Os and marrow are highly vascularised and account for approximately 10-20% of cardiac output (Bartl and Bartl, 2017). Blood vessels in bone are necessary for nearly all skeletal functions, including the delivery of oxygen and nutrients, homoeostasis and repair (Tomlinson and Silva, 2013). The blood supply in long bones is derived from the nutrient artery and the periosteal, epiphyseal and metaphyseal arteries (Iyer, 2019).
Each avenue is also accompanied by nerve fibres, which co-operative into the marrow cavities. Arteries are the main source of blood and nutrients for long basic, entering through the nutrient foramen, and so dividing into ascending and descending branches. The ends of long bones are supplied by the metaphyseal and epiphyseal arteries, which arise from the arteries from the associated articulation (Bartl and Bartl, 2017).
If the claret supply to bone is disrupted, information technology can result in the death of bone tissue (osteonecrosis). A common case is following a fracture to the femoral neck, which disrupts the claret supply to the femoral head and causes the bone tissue to become necrotic. The femoral head structure then collapses, causing pain and dysfunction.
Growth
Bones begin to form in utero in the get-go eight weeks post-obit fertilisation (Moini, 2019). The embryonic skeleton is starting time formed of mesenchyme (connective tissue) structures; this primitive skeleton is referred to as the skeletal template. These structures are then developed into bone, either through intramembranous ossification or endochondral ossification (replacing cartilage with bone).
Bones are classified according to their shape (Box 1). Flat basic develop from membrane (membrane models) and sesamoid basic from tendon (tendon models) (Waugh and Grant, 2018). The term intra-membranous ossification describes the direct conversion of mesenchyme structures to bone, in which the fibrous tissues become ossified equally the mesenchymal stem cells differentiate into osteoblasts. The osteoblasts then start to lay down bone matrix, which becomes ossified to course new bone.
Box 1. Types of bones
Long bones – typically longer than they are wide (such equally humerus, radius, tibia, femur), they contain a diaphysis (shaft) and epiphyses at the distal and proximal ends, joining at the metaphysis. In growing os, this is the site where growth occurs and is known equally the epiphyseal growth plate. Well-nigh long bones are located in the appendicular skeleton and function as levers to produce movement
Curt bones – pocket-size and roughly cube-shaped, these contain mainly cancellous os, with a thin outer layer of cortical bone (such every bit the bones in the easily and tarsal bones in the feet)
Flat bones – sparse and normally slightly curved, typically containing a thin layer of cancellous bone surrounded by cortical bone (examples include the skull, ribs and scapula). Most are located in the axial skeleton and offering protection to underlying structures
Irregular basic – bones that practise not fit in other categories because they have a range of different characteristics. They are formed of cancellous bone, with an outer layer of cortical bone (for example, the vertebrae and the pelvis)
Sesamoid basic – round or oval bones (such as the patella), which develop in tendons
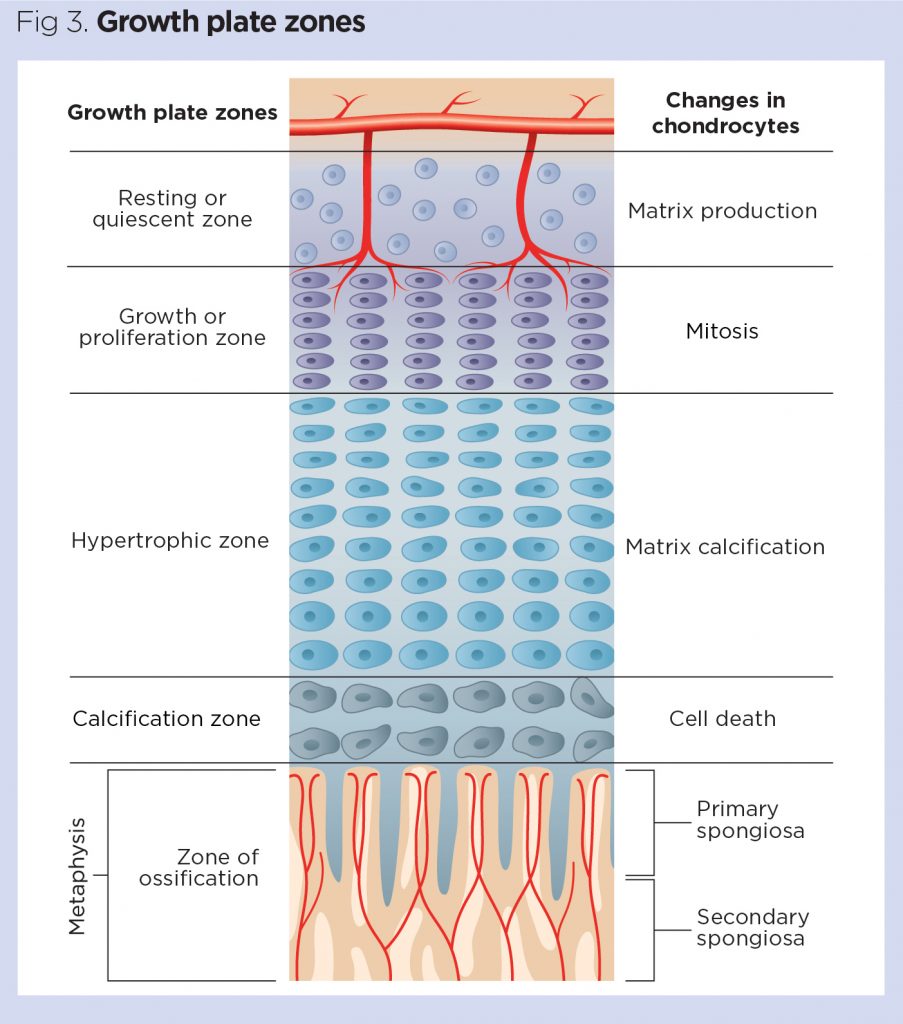
Long, brusk and irregular bones develop from an initial model of hyaline cartilage (cartilage models). Once the cartilage model has been formed, the osteoblasts gradually replace the cartilage with bone matrix through endochondral ossification (Robson and Syndercombe Court, 2018). Mineralisation starts at the centre of the cartilage construction, which is known every bit the chief ossification centre. Secondary ossification centres besides grade at the epiphyses (epiphyseal growth plates) (Danning, 2019). The epiphyseal growth plate is composed of hyaline cartilage and has four regions (Fig iii):
Resting or quiescent zone – situated closest to the epiphysis, this is composed of small scattered chondrocytes with a low proliferation rate and anchors the growth plate to the epiphysis;
Growth or proliferation zone – this area has larger chondrocytes, arranged similar stacks of coins, which split up and are responsible for the longitudinal growth of the bone;
Hypertrophic zone – this consists of large maturing chondrocytes, which migrate towards the metaphysis. There is no new growth at this layer;
Calcification zone – this last zone of the growth plate is only a few cells thick. Through the process of endochondral ossification, the cells in this zone become ossified and form function of the 'new diaphysis' (Tortora and Derrickson, 2009).
Basic are not fully developed at birth, and proceed to form until skeletal maturity is reached. By the cease of adolescence around ninety% of adult bone is formed and skeletal maturity occurs at effectually xx-25 years, although this tin vary depending on geographical location and socio-economical conditions; for example, malnutrition may delay bone maturity (Drake et al, 2019; Bartl and Bartl, 2017). In rare cases, a genetic mutation can disrupt cartilage development, and therefore the development of bone. This tin result in reduced growth and brusque stature and is known every bit achondroplasia.
The human being growth hormone (somatotropin) is the main stimulus for growth at the epiphyseal growth plates. During puberty, levels of sexual activity hormones (oestrogen and testosterone) increment, which stops prison cell sectionalization inside the growth plate. Every bit the chondrocytes in the proliferation zone stop dividing, the growth plate thins and eventually calcifies, and longitudinal os growth stops (Ralston and McInnes, 2014). Males are on average taller than females because male puberty tends to occur afterwards, so male bones take more time to grow (Waugh and Grant, 2018). Over-secretion of human being growth hormone during childhood can produce gigantism, whereby the person is taller and heavier than ordinarily expected, while over-secretion in adults results in a condition called acromegaly.
If there is a fracture in the epiphyseal growth plate while bones are still growing, this can after inhibit bone growth, resulting in reduced bone formation and the os existence shorter. It may as well cause misalignment of the joint surfaces and cause a predisposition to developing secondary arthritis afterward in life. A discrepancy in leg length tin lead to pelvic obliquity, with subsequent scoliosis caused by trying to compensate for the difference.
Remodelling
Once bone has formed and matured, information technology undergoes constant remodelling by osteoclasts and osteoblasts, whereby erstwhile bone tissue is replaced by new bone tissue (Fig iv). Bone remodelling has several functions, including mobilisation of calcium and other minerals from the skeletal tissue to maintain serum homoeostasis, replacing onetime tissue and repairing damaged bone, as well as helping the body accommodate to unlike forces, loads and stress applied to the skeleton.
Calcium plays a significant role in the body and is required for muscle contraction, nerve conduction, cell division and blood coagulation. Every bit only i% of the torso'southward calcium is in the blood, the skeleton acts as storage facility, releasing calcium in response to the body's demands. Serum calcium levels are tightly regulated past two hormones, which work antagonistically to maintain homoeostasis. Calcitonin facilitates the deposition of calcium to bone, lowering the serum levels, whereas the parathyroid hormone stimulates the release of calcium from bone, raising the serum calcium levels.
Osteoclasts are large multinucleated cells typically found at sites where there is active bone growth, repair or remodelling, such every bit around the periosteum, inside the endosteum and in the removal of calluses formed during fracture healing (Waugh and Grant, 2018). The osteoclast prison cell membrane has numerous folds that confront the surface of the bone and osteoclasts pause down os tissue by secreting lysosomal enzymes and acids into the space between the ruffled membrane (Robson and Syndercombe Court, 2018). These enzymes dissolve the minerals and some of the bone matrix. The minerals are released from the os matrix into the extracellular infinite and the rest of the matrix is phagocytosed and metabolised in the cytoplasm of the osteoclasts (Bartl and Bartl, 2017). In one case the area of bone has been resorbed, the osteoclasts motion on, while the osteoblasts move in to rebuild the bone matrix.
Osteoblasts synthesise collagen fibres and other organic components that make upward the bone matrix. They likewise secrete alkali metal phosphatase, which initiates calcification through the deposit of calcium and other minerals around the matrix (Robson and Syndercombe Court, 2018). As the osteoblasts deposit new bone tissue effectually themselves, they go trapped in pockets of bone chosen lacunae. Once this happens, the cells differentiate into osteocytes, which are mature bone cells that no longer secrete bone matrix.
The remodelling process is accomplished through the counterbalanced activity of osteoclasts and osteoblasts. If bone is built without the appropriate balance of osteocytes, information technology results in abnormally thick bone or bony spurs. Conversely, too much tissue loss or calcium depletion can pb to frail bone that is more than susceptible to fracture. The larger surface expanse of cancellous bones is associated with a college remodelling rate than cortical bone (Bartl and Bartl, 2017), which means osteoporosis is more evident in bones with a high proportion of cancellous bone, such as the head/cervix of femur or vertebral bones (Robson and Syndercombe Court, 2018). Changes in the remodelling rest may as well occur due to pathological conditions, such as Paget's disease of bone, a status characterised past focal areas of increased and disorganised os remodelling affecting one or more bones. Typical features on Ten-ray include focal patches of lysis or sclerosis, cortical thickening, disorganised trabeculae and trabecular thickening.
As the torso ages, bone may lose some of its force and elasticity, making it more susceptible to fracture. This is due to the loss of mineral in the matrix and a reduction in the flexibility of the collagen.
Diet and lifestyle factors
Adequate intake of vitamins and minerals is essential for optimum bone formation and ongoing os health. Ii of the most important are calcium and vitamin D, but many others are needed to keep bones strong and healthy (Box two).
Box ii. Vitamins and minerals needed for bone health
Primal nutritional requirements for bone wellness include minerals such equally calcium and phosphorus, as well as smaller qualities of fluoride, manganese, and fe (Robson and Syndercombe Court, 2018). Calcium, phosphorus and vitamin D are essential for effective bone mineralisation. Vitamin D promotes calcium absorption in the intestines, and deficiency in calcium or vitamin D can predispose an individual to ineffective mineralisation and increased take a chance of developing weather such equally osteoporosis and osteomalacia.
Other key vitamins for salubrious bones include vitamin A for osteoblast function and vitamin C for collagen synthesis (Waugh and Grant, 2018).
Physical practice, in particular weight-bearing practice, is important in maintaining or increasing os mineral density and the overall quality and strength of the bone. This is because osteoblasts are stimulated past load-bearing practice and and then bones subjected to mechanical stresses undergo a higher charge per unit of bone remodelling. Reduced skeletal loading is associated with an increased chance of developing osteoporosis (Robson and Syndercombe Court, 2018).
Conclusion
Bones are an important part of the musculoskeletal system and serve many core functions, as well as supporting the body's structure and facilitating movement. Bone is a dynamic structure, which is continually remodelled in response to stresses placed on the body. Changes to this remodelling procedure, or inadequate intake of nutrients, tin can result in changes to os construction that may predispose the torso to increased gamble of fracture. Part 2 of this series will review the structure and function of the skeletal organization.
Key points
- Bones are cardinal to providing the trunk with structural support and enabling move
- Nearly of the trunk's minerals are stored in the bones
- Diet and lifestyle tin can affect the quality of os formation
- Afterward bones have formed they undergo constant remodelling
- Changes in the remodelling procedure tin can result in pathology such as Paget's disease of bone or osteoporosis
References
Bartl R, Bartl C (2017) Construction and compages of bone. In: Bone Disorder: Biology, Diagnosis, Prevention, Therapy.
Danning CL (2019) Structure and part of the musculoskeletal organisation. In: Banasik JL, Copstead L-EC (eds) Pathophysiology. St Louis, MO: Elsevier.
Drake RL et al (eds) (2019) Gray's Beefcake for Students. London: Elsevier.
Iyer KM (2019) Anatomy of bone, fracture, and fracture healing. In: Iyer KM, Khan WS (eds) Full general Principles of Orthopedics and Trauma. London: Springer.
Moini J (2019) Bone tissues and the skeletal system. In: Anatomy and Physiology for Health Professionals. Burlington, MA: Jones and Bartlett.
Ralston SH, McInnes IB (2014) Rheumatology and bone illness. In: Walker BR et al (eds) Davidson's Principles and Do of Medicine. Edinburgh: Churchill Livingstone.
Robson Fifty, Syndercombe Court D (2018) Bone, musculus, skin and connective tissue. In: Naish J, Syndercombe Courtroom D (eds) Medical Sciences. London: Elsevier
Tomlinson RE, Silva MJ (2013) Skeletal blood catamenia in bone repair and maintenance. Os Inquiry; one: 4, 311-322.
Tortora GJ, Derrickson B (2009) The skeletal system: bone tissue. In: Principles of Beefcake and Physiology. Chichester: John Wiley & Sons.
Waugh A, Grant A (2018) The musculoskeletal system. In: Ross & Wilson Anatomy and Physiology in Health and Illness. London: Elsevier.
Source: https://www.nursingtimes.net/clinical-archive/orthopaedics/skeletal-system-1-the-anatomy-and-physiology-of-bones-27-01-2020/
0 Response to "Scientific Baby Bone Pictures Bone Anatomy From Birth to Deatb"
Kommentar veröffentlichen